Disease of the Month – Psoriatic arthritis
Shots:
- Psoriatic arthritis is a chronic inflammatory condition characterized by joint pain, stiffness and swelling
- In this reprise of our Disease of the Month report, we present an enlightening description of Psoriatic arthritis with a thorough study of epidemiology, market size, disease management, potential medicines, patient advocacy groups, and the key players involved
- For a deep dive landscape, reach out to us at connect@pharmashots.com
Psoriatic arthritis is a chronic autoimmune disease that causes joint inflammation and is characterized by psoriasis, a condition that leads to a red, scaly rash. It can affect any joint and cause pain, stiffness, and swelling. It typically occurs in people with psoriasis, though the severity of skin and joint symptoms can vary.
Types of Psoriatic Arthritis 1,2
Psoriatic arthritis can be classified according to which joints are affected, or which side of the body exhibits symptoms. There are five distinct types of psoriatic arthritis:
-
Distal Interphalangeal Predominant Psoriatic Arthritis: Affects joints close to fingers and toes. It is more likely to develop nail psoriasis
-
Symmetric Polyarthritis: Affects >5 joints on both sides of the body. For example, affecting both the ankles, shoulders & elbows
-
Asymmetric Oligoarticular: Affects 2-4 different joints on each body side. For example, one ankle & one shoulder
-
Spondylitis: Affects joints between the vertebrae in the spine
-
Arthritis Mutilans: A rare and severe type of Psoriatic arthritis that causes inflammation in the hands & feet, resulting in bone loss & joint deformities
Symptoms: 3,4
Symptoms of psoriatic arthritis can vary from person to person. Some of the common symptoms are:
1. Joint Symptoms:
- Pain and swelling in the joints, often in fingers, toes, wrists, knees, or ankles
- Morning stiffness in the affected joints
- Sausage-like swelling in the fingers and toes (dactylitis)
- Pain and tenderness in the tendons (enthesitis), commonly in the Achilles tendon or around the elbows
- Back pain if the spine is affected (spondylitis)
2. Skin Symptoms:
- Psoriasis is often present, which includes red, scaly patches of skin on the scalp, elbows, or knees
- Nail changes like pitting, ridging, or separation from the nail bed
3. Other Symptoms:
- Eye Inflammation: Includes uveitis and inflammation in the eye’s middle layer, leading to eye pain, redness & blurry vision
- Fatigue or weakness
- Inflammatory Bowel Disease: characterized by inflammation in the digestive tract
Comorbidities: People with PsA are at higher risk of developing high blood pressure (hypertension), high cholesterol (hyperlipemia), obesity, diabetes, depression, anemia, and muscle weakness.
Causes: 3,4
-
Genetics: A person with a family history may develop PsA
-
Environmental Factors: Stress, obesity, infections, and injuries can trigger the disease
Diagnosis: 4,5
There is no definitive test to diagnose PsA. However, certain tests can help exclude other conditions that cause joint pain, like rheumatoid arthritis or gout.
- Physical Examination: Checking joints for signs of swelling or tenderness; fingernails for pitting, flaking & other abnormalities; and press soles of the feet and around heels to identify tender areas
- Imaging Tests: X-rays and MRIs to assess joint damage
- Laboratory Tests:
- Rheumatoid factor (RF): Rheumatoid factor (RF) is an antibody commonly found in the blood of people with rheumatoid arthritis but not in PsA. Testing for RF can help differentiate between the two conditions
- Joint Fluid Test: Fluid from an affected joint, often the knee, is examined for uric acid crystals which indicates gout rather than psoriatic arthritis. It's also possible to have both conditions
Management and Treatment: 5,1
Currently, PsA has no cure, but its symptoms can be managed through available treatment
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs are given to relieve pain. NSAIDs that can be taken without a prescription are ibuprofen (Advil, Motrin IB, others) & naproxen sodium (Aleve)
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs slow disease progression. Some of the commonly used DMARDs are methotrexate (Trexall, Otrexup, others), leflunomide (Arava) & sulfasalazine (Azulfidine)
- Immunosuppressants: To suppress the immune system
- Biologics Agents: Biologics (TNF inhibitors, IL-17 inhibitors) for more severe cases, such as adalimumab (Humira), certolizumab (Cimzia), etc
- Enzyme Inhibitors: Drugs that block specific enzymes, such as PDE-4, to decrease inflammation
- Steroid injections: To reduce joint inflammation but is usually not recommended as it worsens skin rash
- Joint replacement surgery: Severely damaged joints can be replaced with artificial ones made of metal and plastic
Epidemiology: 6
- Prevalence: PsA affects about 0.05% to 0.25% of the global population. Among people with psoriasis, 6% to 41% develop PsA
- Age of Onset: It typically occurs between the age group 30-40
- Gender: PsA affects both men and women equally
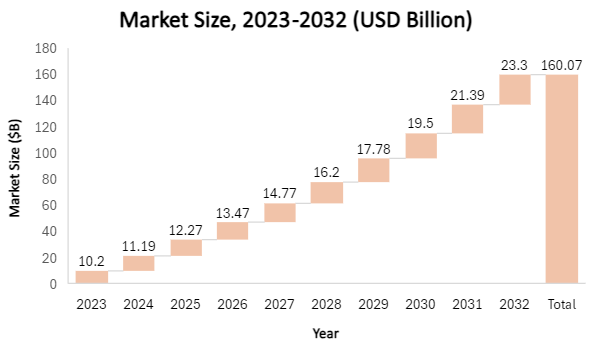
Market size: 7
In 2023, the global PsA treatment market size was valued at $10.2B and is estimated to reach $23.3B by 2032 registering a CAGR growth of 9.7% between 2024 and 2032
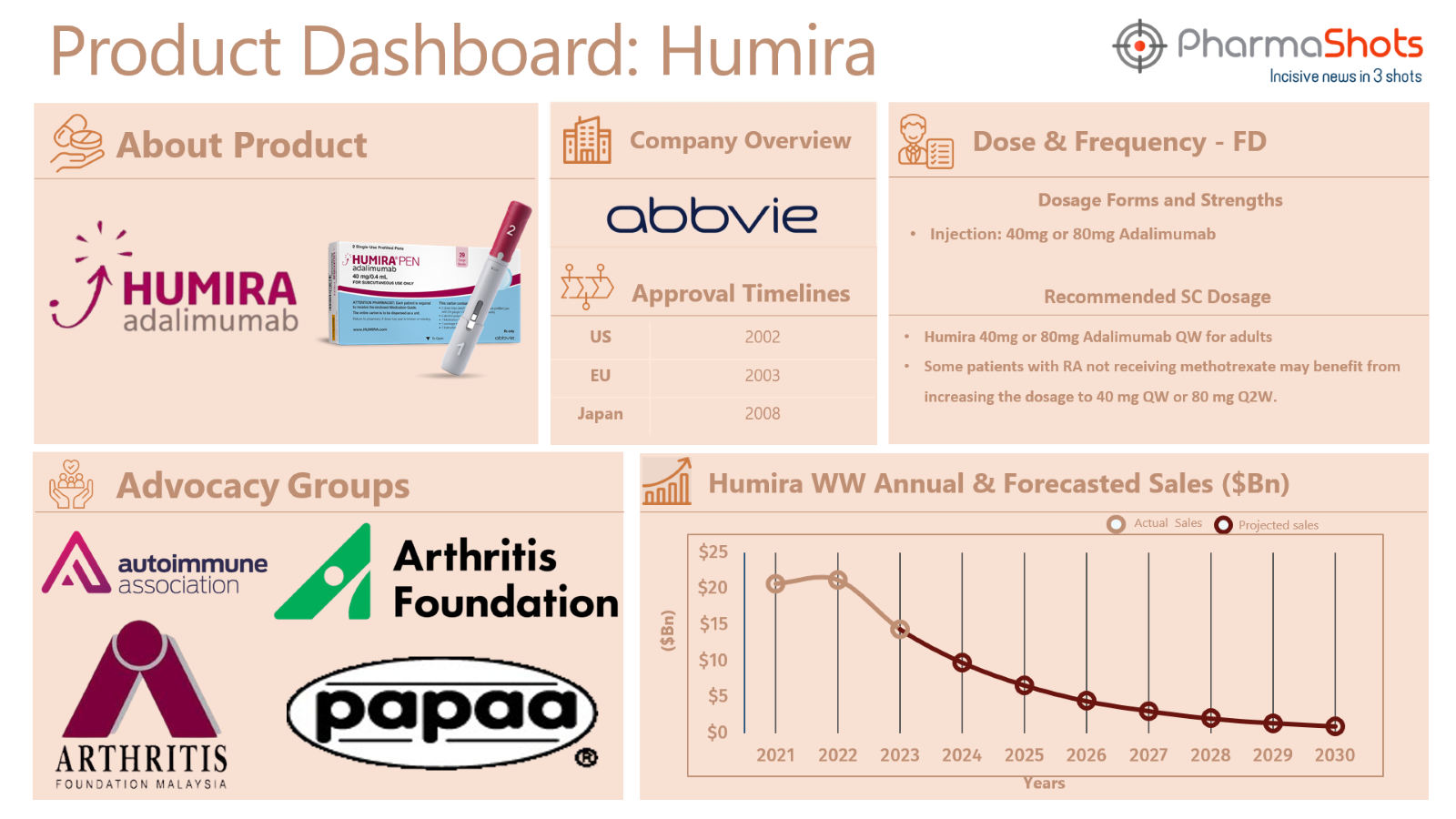
Product Dashboard 8
Humira (adalimumab) is indicated for the treatment of Psoriatic Arthritis (PsA)
Key Players in the Market
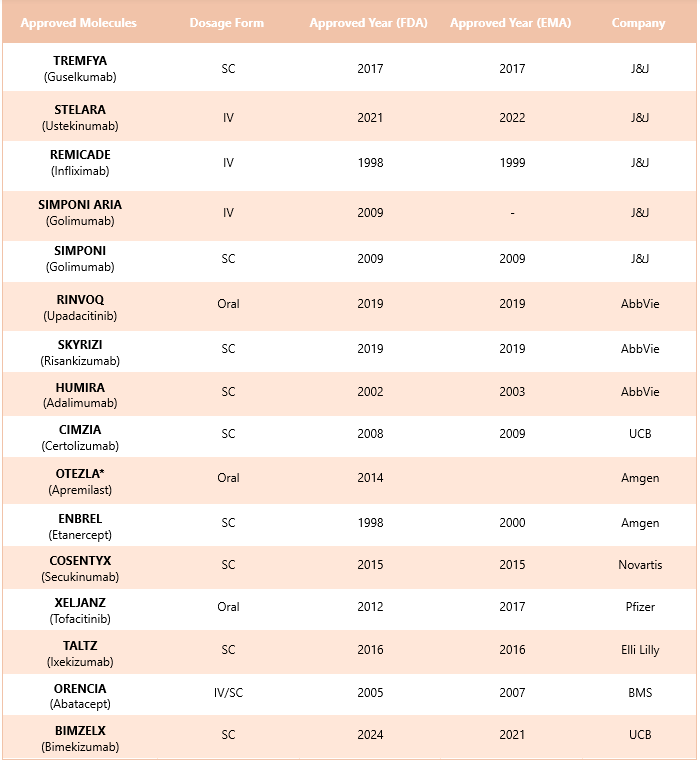
Note: *CHMP Positive Opinion in __2024
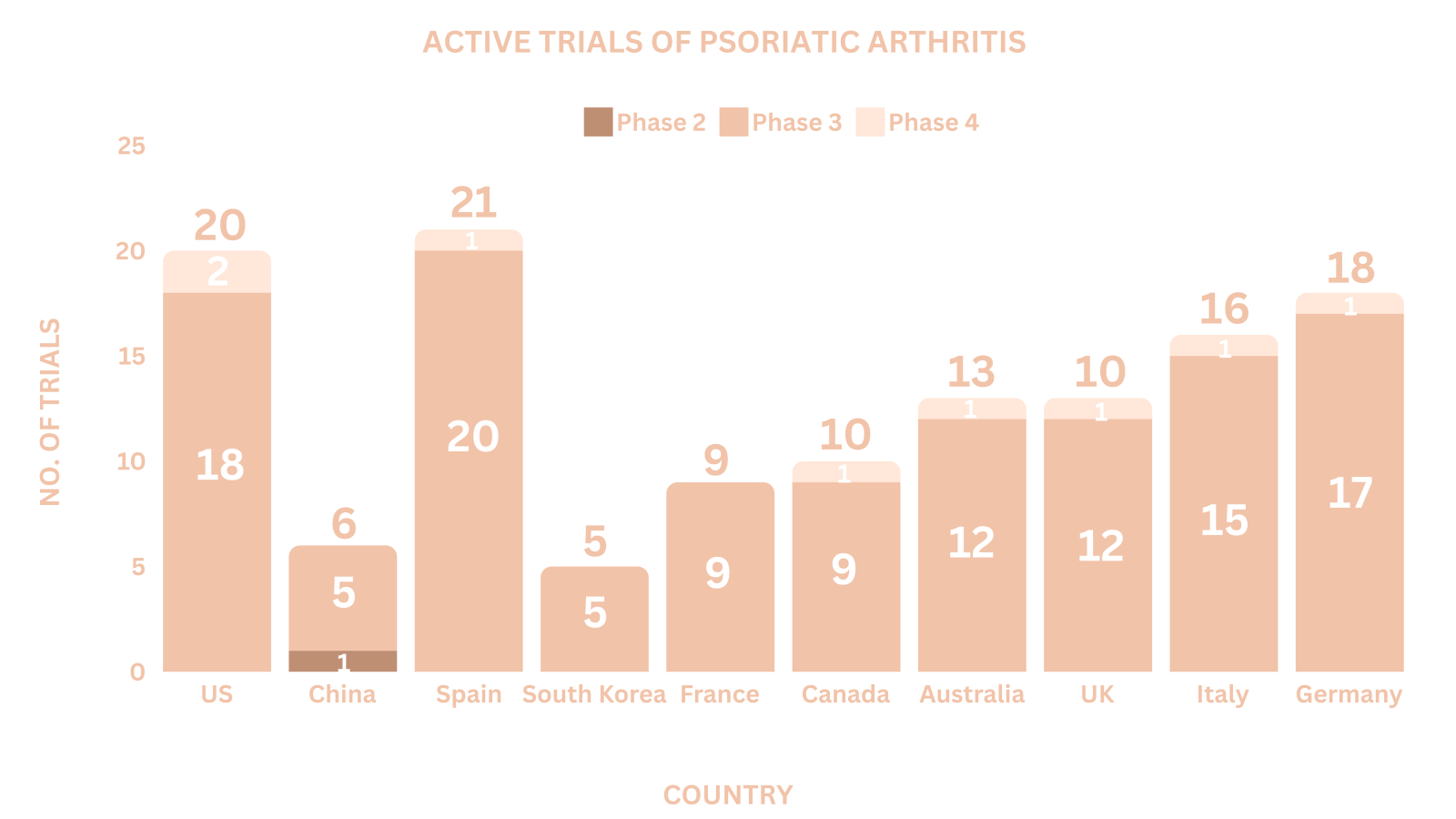
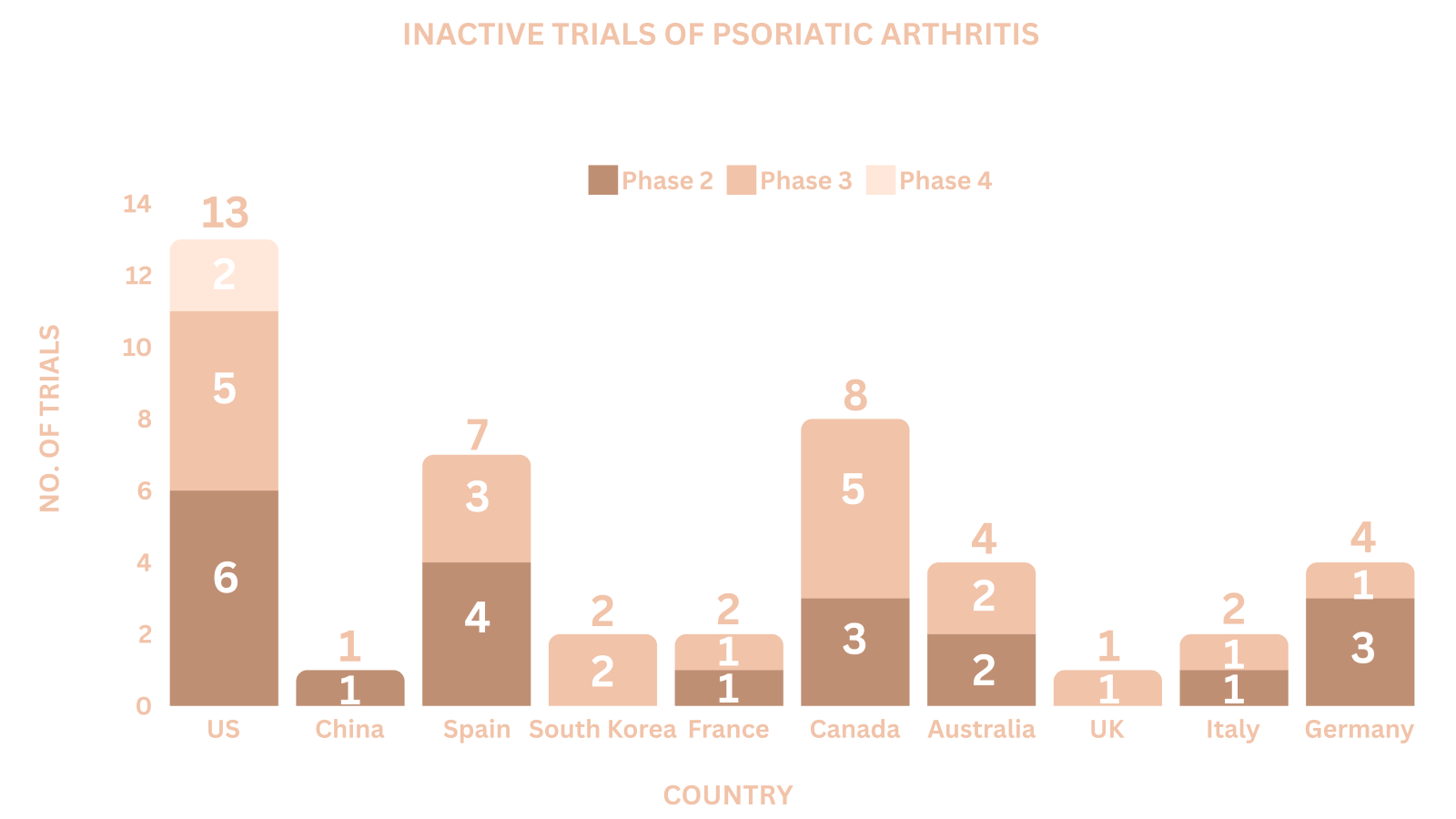
Clinical Trial Analysis 9
Based on the geographical distribution, the interventional and industry-sponsored clinical trials are classified in the below-mentioned graph into two groups based on their status: Active (recruiting; active, not recruiting; not yet recruiting; enrolling by invitation and suspended) and Inactive (withdrawn; terminated and trials with unknown status)
The maximum number of active trials is being conducted across the US followed by Spain and Italy (as represented in the graph)
Note:
-
The number of trials were extracted on Sep 30, 2024.
-
These Clinical Trials also Include Biosimilars.
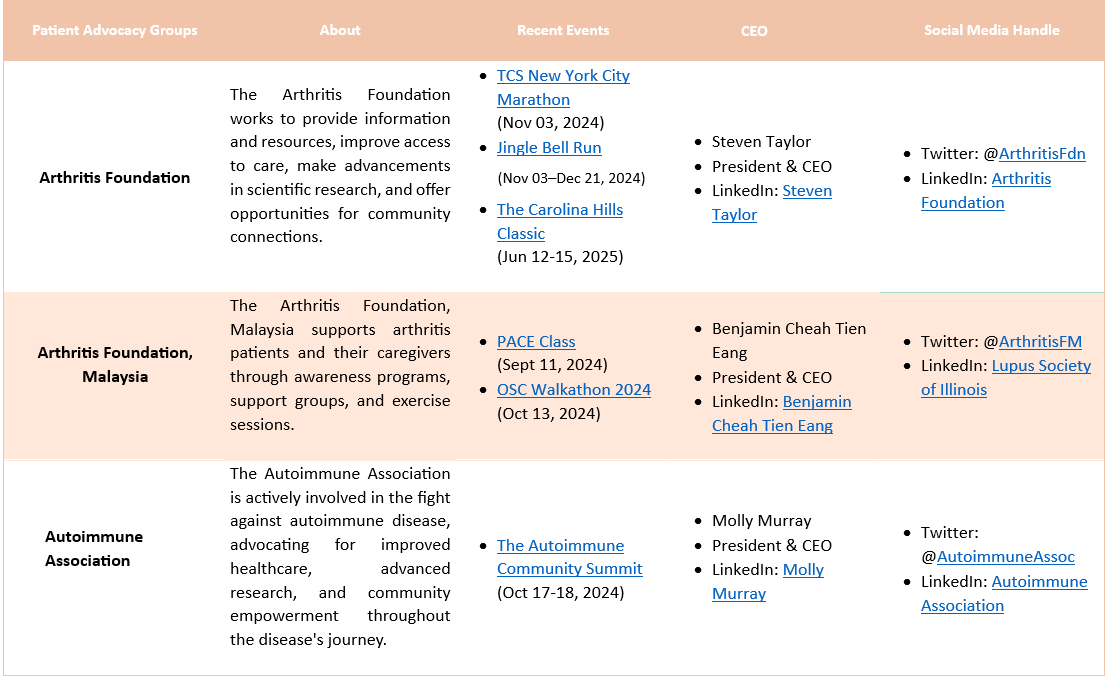
Patient Advocacy Groups (PAGs) for Psoriatic Arthritis
Several advocacy groups are working steadfastly to help improve the lives of patients with Psoriatic Arthritis
Patient Stories 10
-
Dominic Wong (Age: 49)
My name is Dom, and I was diagnosed with Psoriasis in 2003 at age 28. My experience started with fatigue; the pain came about 3 months after. I was on a holiday and I was extremely tired after breakfast. I told my family I had to rest and sleep in. I was once told my doctor, that if you are on holiday and you feel extremely tired – you may want to speak to your doctor to pursue a medical investigation.
After consulting my dermatologist, I was advised to see a rheumatologist. The rheumatologist recommended further checks with other specialists to rule out other conditions. I went to consult with a Cardiologist, Endocrine Specialist, Neurologist, ENT Specialist, Immunologist and finally back to see the Rheumatologist. During this medical investigation. I had to further consult the ENT and sleep dentist due to being diagnosed with sleep apnea (a known comorbidity). The entire journey of going from doctor to doctor took about 1 year.
I pursued the above medical consultations via the private medical care route as this was during the pandemic. I wanted to get the fastest diagnosis possible and to choose the doctors based on their experience.
I am currently using biologics to manage my PsA. For now, the pain has been in remission. Fatigue remains my symptomatic challenge as there are days when this symptom is very troublesome.
Living with the disease through my lived experience and via the lens of 2 other friends from the Psoriasis Association of Malaysia (PAM)
As I was just diagnosed recently – I was advised to start early effective intervention to ensure that the disease can be slowed down. The objective is to stop or delay the in-body inflammation that damages our spine, joints, and other areas. I asked my doctor, given effective medication – is there any expectation of what will be the state of my illness in 5 or 10 years? My rheumatologist did say he can’t give me a prediction. They can only monitor my health and symptoms over time to see the illness’s progression.
Source: https://www.afm.org.my/2023/05/05/psoriatic-arthritis-psa-patient-mr-dominic-wong-shui-foong/
References:
- WebMD
- MedLine Plus
- Niams.Nih
- My Cleveland Clinic
- Mayo Clinic
- Ncbi.nlm
- GMI Insights
- Humira PI
- CT.Gov
- Patient Story
Related Post: Systemic Lupus Erythematosus
Tags

A passionate content writer with expertise in delivering high-quality and engaging content, Dipanshu is a keen reader and a versatile writer. Dipanshu dedicatedly covers news ranging from biopharma, life sciences, biotech, and MedTech to diagnostics and animal health companies, FDA, EMA, and biosimilar approvals. He can be contacted at connect@pharmashots.com